When I got my diagnosis, I really couldn’t wrap my head
around what leukemia was. I had no idea that it was a blood cancer, and I certainly
had no idea that treating this bastard was such a long-term affair. There have been of myriad of complicated,
interrelated details that boggle the imagination, literally hundreds of medical
and support staff rotating from one organization (within the VA system and
other institutions), thousands of shiny, jagged pills, IVs, syringes, scans,
probes, swabs, tests, biopsies, consults, and so much more. How does anyone
keep track of it all? The simple answer is not that I have to rise to the
occasion, but rather work together with them all and my caregiving team to make
it work. No one can do this solo. Just ain’t
no way, my friend!
I thought what I’d do today is give you a guided tour of what a routine day is like to give you an idea of all the people involved as well as some context of what life is like. It’s very much like an inpatient day except that I get to leave when the doctors give me the OK that I’m still healthy and self-sufficient to be an outpatient at the end of each day. It’s obviously a big bonus for the little things like choosing what kind of food you want to eat, sleeping in a bed that is more comfortable and not getting awakened or interrupted by someone wanting to poke, prod, or otherwise molest you at any given hour! Yeah, big bonus there. Remember, I have a great soft spot for nurses, but checking my vitals at 1:00 a.m. when I’m actually sleeping? Ah, yeah, those were the days…and hopefully not to be repeated any time soon.
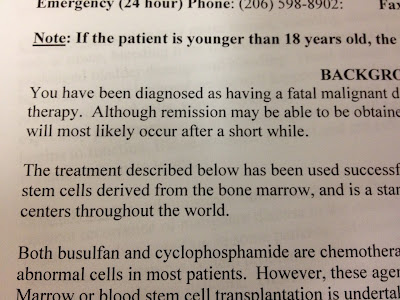
The bone marrow transplant process is nothing short of a chemical miracle in my mind. It’s hard for me to really grasp the significance of this little bag of someone else’s stem cells being infused into my arm being fruitful and multiplying into enough of a life-saving force to engraft to my own body and be formidable enough to fight off any remaining leukemia that might be in my system after that lovely toxic chemical goodness has done its good and perfect work on decimating my own immune system…yet it is and it has! It is a truly drastic and extreme life-saving measure and as I was told before I got here, I would be taken to death’s door and brought back. Once again, I was quite literally there and I’m back and working through the process toward restoration and healing.
The transplant process here has a rough timeline that takes about 100 days, some more, some less depending on how one’s body reacts to all the pharmacopeia and of course the transplant itself – and there is a whole mess of it every day to keep on top of. Day 1 is actually the day one receives the stem cells even though the treatment begins before getting them. There are variations on the transplant depending on who provides the stem cells. An “autologous” transplant, for example is where the patient provides his or her own stem cells for later use while those like me who needed a donor receive an “allogeneic” transplant. Then there are two subsets of each of these – a mini or a full myeloablative transplant. I had “the full monty” as people were calling it because of my younger age and ability to withstand the more arduous process. Trust me, it was indeed an arse-kicker, but there should be fewer complications down the line and I skirted the one key part of treatment that I just couldn’t reconcile: total body irradiation.
So, 42 days of inpatient fun later, I was discharged to be on outpatient treatment. What, you may ask, do I do during these days post-transplant at the hospital each day? Let’s begin with my virtual tour from the fabulous Marriott Towneplace Suites in Renton, WA! The VA puts my sons and me up in a two-bedroom suite with a small kitchenette. It’s a comfortable space and the people here have taken good care of us, but you all know we’d rather be home…not a bad home away from home considering the circumstances.
My day starts with taking care of one of the side effects of
the high dose of steroids I’ve been prescribed – monitoring and correcting for
high blood sugar. And no, dear ones, they’re not that kind of steroids. If
anything, they do the exact opposite and are eating away my muscle so I have to
be mindful to be active. Someone had posted on my Facebook page that with all the weight I was losing and the steroids, I'd be ripped when I came back. I can only wish. But, in my case, just like a diabetic, I get to inject myself with insulin four times a
day as the steroids throw my blood sugar through the roof. Before treatment, my
blood glucose levels were absolutely normal. For now, I get to poke my fingers
to test for blood sugar levels and then based on how high the numbers are inject
myself with the appropriate amount of insulin before each meal and before bed.
Lovely way to start the day, huh? I also check my blood pressure and
temperature and I’m eating quite a bit differently than I might have otherwise.
This is truly an education in nutrition and self-control as well as the medical side of things
as we go along. I thought what I’d do today is give you a guided tour of what a routine day is like to give you an idea of all the people involved as well as some context of what life is like. It’s very much like an inpatient day except that I get to leave when the doctors give me the OK that I’m still healthy and self-sufficient to be an outpatient at the end of each day. It’s obviously a big bonus for the little things like choosing what kind of food you want to eat, sleeping in a bed that is more comfortable and not getting awakened or interrupted by someone wanting to poke, prod, or otherwise molest you at any given hour! Yeah, big bonus there. Remember, I have a great soft spot for nurses, but checking my vitals at 1:00 a.m. when I’m actually sleeping? Ah, yeah, those were the days…and hopefully not to be repeated any time soon.
The bone marrow transplant process is nothing short of a chemical miracle in my mind. It’s hard for me to really grasp the significance of this little bag of someone else’s stem cells being infused into my arm being fruitful and multiplying into enough of a life-saving force to engraft to my own body and be formidable enough to fight off any remaining leukemia that might be in my system after that lovely toxic chemical goodness has done its good and perfect work on decimating my own immune system…yet it is and it has! It is a truly drastic and extreme life-saving measure and as I was told before I got here, I would be taken to death’s door and brought back. Once again, I was quite literally there and I’m back and working through the process toward restoration and healing.
The transplant process here has a rough timeline that takes about 100 days, some more, some less depending on how one’s body reacts to all the pharmacopeia and of course the transplant itself – and there is a whole mess of it every day to keep on top of. Day 1 is actually the day one receives the stem cells even though the treatment begins before getting them. There are variations on the transplant depending on who provides the stem cells. An “autologous” transplant, for example is where the patient provides his or her own stem cells for later use while those like me who needed a donor receive an “allogeneic” transplant. Then there are two subsets of each of these – a mini or a full myeloablative transplant. I had “the full monty” as people were calling it because of my younger age and ability to withstand the more arduous process. Trust me, it was indeed an arse-kicker, but there should be fewer complications down the line and I skirted the one key part of treatment that I just couldn’t reconcile: total body irradiation.
So, 42 days of inpatient fun later, I was discharged to be on outpatient treatment. What, you may ask, do I do during these days post-transplant at the hospital each day? Let’s begin with my virtual tour from the fabulous Marriott Towneplace Suites in Renton, WA! The VA puts my sons and me up in a two-bedroom suite with a small kitchenette. It’s a comfortable space and the people here have taken good care of us, but you all know we’d rather be home…not a bad home away from home considering the circumstances.
 |
| From the front of the Seattle VA Hospital - As much time as I spend here, it feels like home away from home...except that it isn't. It's actually quite the sprawling complex behind this façade. |
After a quick shower, I run over to our hotel continental
breakfast and grab a quick bite and take about 20 different pills for various
things including liver, kidney, electrolyte, and immuno-suppressant functions.
Anti-rejection drugs come along later in the day after my blood draw at the
hospital.
Off to the hospital in the characteristic rain and we are
typically on the surface route instead of the Interstate. The traffic going
toward the city isn’t unlike my memories of SoCal, but not quite as many lanes
to accommodate all the many cars. I won’t
take the time to criticize Seattle drivers, but I will say they’re a lot nicer
face-to-face. Let’s leave it at that.
At the hospital, it’s back to the Bone Marrow Transplant Unit where it feels like a family and Cheers where everybody knows your name. There, we take our turns in the outpatient room, getting our routine blood draws and the IVs that are on our treatment plan. In the picture here, I’m getting my PICC line dressing changed. That’s a weekly occurrence, but it’s painless and it keeps me from getting stuck with a regular IV needle every time I come in, so while it really hurt going in, it has saved me a huge amount of discomfort over the months in getting blood draws and IVs otherwise. Other patients get something called a Hickman port which is essentially the same thing I have except it is installed over the chest and has three “lumens” or ports instead of my two. Since I was an allogeneic patient, I didn’t need the Hickman. The amount of time we spend in the outpatient room can vary on the number of different treatments we need during the day. For me, it’s routinely two hour-long IVs, the blood draw, and occasionally, I get something else. By the time I’m done, it’s about noon. The lab turns around the blood chemistry results pretty quickly and we’ve all been taught what to look for.
During this time as well, and more to the point of why we
come in each day is to see the attending physician and his coterie to again,
make sure I’m on the up-and-up and moving along according to plan. These visits
are essentially identical to ‘rounds’ that these same doctors do if I were
inpatient. He has with him, the most current hem/onc fellow, a staff
pharmacist, the outpatient nurse, nutritionist, and a few others that don’t
identify themselves. They pepper me with
questions on how I’m doing, check my mouth for sores, listen to my lungs, check
for edema in my legs, and make some small talk. At this point, it feels very
cordial, but it’s not unusual after these sessions to get a call to adjust
medication by a little bit or to get additional appointments to ensure
peripheral issues aren’t surfacing. They also interface with other departments
to ensure everyone is on the same page. It’s actually pretty amazing all that
happens between everyone.
At some point during this process, I get “discharged” to go home again. There’s a collective sigh and exodus by all of us outpatients when it happens as it is a legal sort of thing. If we leave early, it’s essentially something called “AMA” (against medical advice) which is obviously rather serious for a cancer patient under active treatment and everyone gets their hand slapped rather hard. It’s not unusual for us to be held back awaiting medication changes, so we’ve waited several hours. Hey, I’m not sleeping there, so I’m quite all right with it. I try to see others while I’m there to make the best use of our time. They also have a cantina in the basement that makes some pretty good sandwiches for cheap. My son and I have found them to be excellent!
If we can get back on the road by 3:00, we can make it back to our hotel room in decent time without the traffic and will find some way to get out and exercise, even if it’s to walk the mall. Seattle really is a rainy place and I’m cognizant of the sunlight restrictions, so the mall is a good place to get some walking in, at least during the week days. My immune system is such that I need to avoid large crowds, so the weekend when the mall is crowded can be problematic for me.
Evenings are spent with my two sons, although we often tend to be three bachelors in the same room. We are all electronically engaged, but somehow in the moment together. I’ve been trying to make sure we do *something* together each night while I’m connected to my evening IV. We have a completely stocked nurse’s station that has occupied the kitchen table in our apartment as you can see in the photo, replete with three separate IV pumps, syringes for insulin, chemo-safe gloves, saline flush syringes, and a panoply of meds to keep my monster box of pills fully stocked. The fun just never ends…but then again, that’s why we’re here.
At some point during this process, I get “discharged” to go home again. There’s a collective sigh and exodus by all of us outpatients when it happens as it is a legal sort of thing. If we leave early, it’s essentially something called “AMA” (against medical advice) which is obviously rather serious for a cancer patient under active treatment and everyone gets their hand slapped rather hard. It’s not unusual for us to be held back awaiting medication changes, so we’ve waited several hours. Hey, I’m not sleeping there, so I’m quite all right with it. I try to see others while I’m there to make the best use of our time. They also have a cantina in the basement that makes some pretty good sandwiches for cheap. My son and I have found them to be excellent!
If we can get back on the road by 3:00, we can make it back to our hotel room in decent time without the traffic and will find some way to get out and exercise, even if it’s to walk the mall. Seattle really is a rainy place and I’m cognizant of the sunlight restrictions, so the mall is a good place to get some walking in, at least during the week days. My immune system is such that I need to avoid large crowds, so the weekend when the mall is crowded can be problematic for me.
Evenings are spent with my two sons, although we often tend to be three bachelors in the same room. We are all electronically engaged, but somehow in the moment together. I’ve been trying to make sure we do *something* together each night while I’m connected to my evening IV. We have a completely stocked nurse’s station that has occupied the kitchen table in our apartment as you can see in the photo, replete with three separate IV pumps, syringes for insulin, chemo-safe gloves, saline flush syringes, and a panoply of meds to keep my monster box of pills fully stocked. The fun just never ends…but then again, that’s why we’re here.
Somewhere along the way, I start to crash, so I give myself
my final injection for the evening and get into bed, only to sleep for about 3
hours at which time I find myself reading for another few hours and try one
more time to get a bit of a nap in before starting over.
It’s a highly-regimented day, so you can imagine how a ‘normal’
day will feel…mostly because you’re living it. We’re about halfway through the
100-day cycle and hope that when December 2 rolls around that the car is headed
eastward on dry roads back to Salt Lake with some happy guys singing campfire
songs (or at least along to the stereo!), so think happy thoughts about my
treatment that it continues to go well and without any hitches along the way.
We’ve had enough to last a lifetime! So for now, one day at a time…hope you enjoyed my abbreviated (even though this was a bit long today) virtual tour of what I’m doing these days.
Be well, stay strong, and as always, much love to you all!
Music for today – Home Life by John Mayer
I think I'm gonna stay home
Have myself a home life
Sitting in the slow-mo
And listening to the daylight
I am not a nomad
I am not a rocket man
I was born a house cat
By the slight of my mother's hand
I think I'm gonna stay home
I want to live in the center of a circle
I want to live on the side of a square
I used to be in my M-Z now
You'll never find me cause my name isn't there
Home life
Been holding out for a home life
My whole life
I want to see the end game
I want to learn her last name
Finish on a Friday
And sit in traffic on the highway
See, I refuse to believe
That my life's gonna be
Just some string of incompletes
Never to lead me to anything remotely close to home life
Been holding out for a home life
My whole life
I can tell you this much
I will marry just once
And if it doesn't work out
Give her half of my stuff
It's fine with me
We said eternity
And I will go to my grave
With the life that I gave
Not just some melody line
On a radio wave
It dissipates
And soon evaporates
But home life doesn't change
I want to live in the center of a circle
I want to live on the side of a square
I'd love to walk to where we can both talk but
I've got to leave you cause my ride is here
Home life
You keep the home life
You take the home life
I'll come back for the home life
I promise
Have myself a home life
Sitting in the slow-mo
And listening to the daylight
I am not a nomad
I am not a rocket man
I was born a house cat
By the slight of my mother's hand
I think I'm gonna stay home
I want to live in the center of a circle
I want to live on the side of a square
I used to be in my M-Z now
You'll never find me cause my name isn't there
Home life
Been holding out for a home life
My whole life
I want to see the end game
I want to learn her last name
Finish on a Friday
And sit in traffic on the highway
See, I refuse to believe
That my life's gonna be
Just some string of incompletes
Never to lead me to anything remotely close to home life
Been holding out for a home life
My whole life
I can tell you this much
I will marry just once
And if it doesn't work out
Give her half of my stuff
It's fine with me
We said eternity
And I will go to my grave
With the life that I gave
Not just some melody line
On a radio wave
It dissipates
And soon evaporates
But home life doesn't change
I want to live in the center of a circle
I want to live on the side of a square
I'd love to walk to where we can both talk but
I've got to leave you cause my ride is here
Home life
You keep the home life
You take the home life
I'll come back for the home life
I promise